Abstract
Background:
Human herpesviruses 6 (HHV-6) A and B cause encephalitis in patients with hematologic malignancies especially those undergoing allogeneic hematopoietic stem cell transplantation (HSCT). Data on the long-term outcomes of patients with HHV-6 encephalitis is limited.
Methods:
To assess the clinical and diagnostic characteristics, and outcomes of patients with HHV-6 encephalitis, we performed a retrospective review of all patients with positive HHV-6 in plasma or CSF between Nov 2011 and Jun 2017. Cases were categorized based on pre-defined criteria for possible, probable and definite HHV-6 encephalitis.
Results:
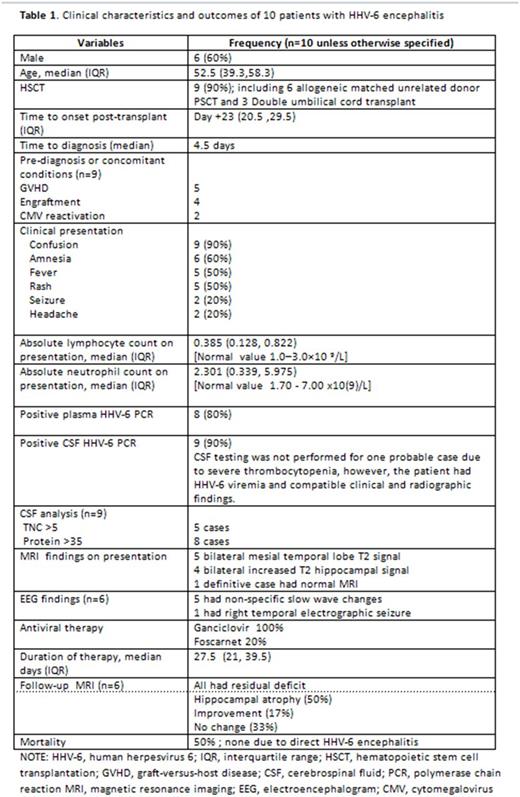
Ten patients with leukemia (n=5), lymphoma (n=2), and other hematologic cancers (n=3) met the criteria for definite (n=8), probable (n=1) and possible (n=1) HHV-6 encephalitis (Table 1). All except one were allogeneic HSCT recipients (three umbilical cord and six matched unrelated donors). Among 9 cases, the median time to onset of illness was early at 23 days (IQR: 20.5-29.5) after transplantation. The clinical symptoms were confusion (80%), retrograde amnesia (60%), fever (50%), rash (50%) and seizures (20%). Before or at the time of illness, patients had GVHD (55%), pre-engraftment syndrome (44%) and CMV (22%). CSF showed mild pleocytosis (WBC 5-22; n=6) and elevated protein (n=8). Plasma HHV-6 PCR was negative in 2 cases, while brain MRI was normal in one definitive case. The most common MRI abnormality was increased T2 signal in the bilateral hippocampal (40%) and mesial temporal lobes (50%). All patients received intravenous ganciclovir for a median duration of 27 days (range: 10-48). Follow-up MRI at 4-40 weeks in 6 patients showed moderate to severe bilateral hippocampal atrophy (50%) or no interval improvement (33%). Five patients died; none were due to HHV-6 encephalitis.
One patient developed possible HHV-6 encephalitis with retinitis at post-transplant day +429; despite clinical improvement, the HHV-6 load remained at >2x106 copies/ml suggesting this case as reactivated chromosomally integrated-HHV-6.
Conclusions:
HHV-6 infection among patients with hematologic malignancies and transplantation is associated with significant long-term morbidity and all-cause mortality. A negative plasma HHV-6 PCR does not rule out the diagnosis. Despite prolonged treatment, persistent neurologic deficits associated with moderate to severe bilateral hippocampal atrophy are characteristic long-term findings.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal